Vitreous Research: The Oxygen Story

Source:http://www.retinalphysician.com/issues/2012/may-2012/vitreous-research-the-oxygen-story
Vitreous Research: The Oxygen Story
Know the role of the vitreous humor to better understand certain ocular pathologies.
PEER REVIEWED
Vitreous Research: The Oxygen Story
Know the role of the vitreous humor to better understand certain ocular pathologies.
Nancy M. Holekamp, MD
| Nancy M. Holekamp, MD, is director of retina services at the Pepose Vision Institute and professor of clinical ophthalmology at Washington University School of Medicine in Saint Louis. She reports no financial interests in any products mentioned in this article. Dr. Holekamp can be reached via e-mail at nholekamp@gmail.com. |
Many retina specialists regard the vitreous body as simply a sticky gel that needs to be removed to fix serious retinal pathology. In other words, the vitreous gel is dispensable. What if, perhaps, we were to ascribe to the vitreous gel a very important physiologic property that was essential to the health of the eye? Would our regard for the vitreous gel change? This article will first present data showing that the vitreous gel does, indeed, perform an important physiological task that is essential to the eye: it consumes oxygen and protects the eye from oxidative damage. The article will then discuss the implications of the vitreous gel having this property only in the gel state and not when liquefied or removed surgically. Specifically, age-related cataract and some cases of primary open-angle glaucoma may be attributed to oxidative damage caused by vitreous liquefaction or vitrectomy surgery. Finally, the potential benefits to the health of the eye of preventing vitreous liquefaction will be proposed.
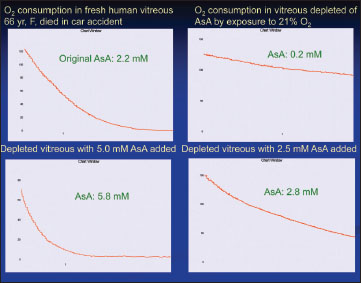
THE VITREOUS GEL CONSUMES OXYGEN
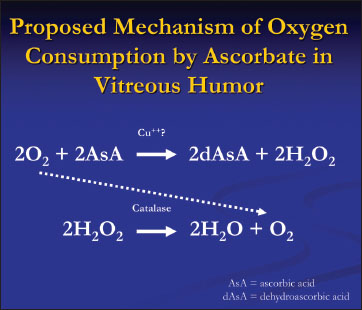
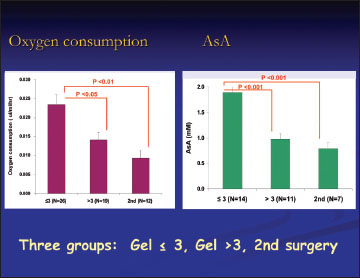
Traditionally the functions of the postnatal vitreous gel have been thought to be biophysical in two ways: (1) to serve as a support structure for the retina, and (2) to serve as a medium for light transmission. Then, in the April 2009 issue of Archives of Ophthalmology, my colleagues at the Washington University School of Medicine and I reported a new and provocative finding: gel vitreous consumes oxygen.1 We performed a series of experiments in which the tip of an oxygen sensor (the size of a 30-gauge needle) was easily fit through trocars at the time of 23- or 25-gauge vitrectomy surgery. In more than 60 patients undergoing vitrectomy surgery for a variety of retinal conditions, we measured intraocular oxygen tension prior to turning on the infusion cannula in two locations: adjacent to the pars plana and in the mid-vitreous cavity. The results were surprising. First, we noted that the inside of the eye exists under hypoxic conditions. The oxygen tension was less than 5% (room air is 21% oxygen). Second, we noted that there was an oxygen gradient in the vitreous cavity. The oxygen tension was higher near the pars plana because of the nearby vascularized tissues, and it was lower in the center of the vitreous cavity.2 If diffusion alone were the only principle at work, then the oxygen tension should have been the same throughout the vitreous cavity. Thus, we hypothesized that the vitreous must actively consume oxygen. This hypothesis led to a series of experiments in which we put cadaver vitreous into an oxygen-impermeable glass tube and placed the oxygen sensor inside. The oxygen tension in the vitreous started out very high, at 120 mm Hg, and within two hours fell to zero. The oxygen tension in the control tube filled with saline remained high at 120 mm Hg. If the cadaver vitreous was stirred overnight in a beaker exposed to room air and then tested the next day, no oxygen consumption occurred. If ascorbate was added to the stirred, air-exposed vitreous, the ability to consume oxygen was restored. If different concentrations of ascorbate were added, the vitreous consumed oxygen at different rates in a linear fashion (Figure 1). Boiling the vitreous did not alter its ability to consume oxygen. The addition of metal chelating agents did not alter the ability of the vitreous to consume oxygen.
THE VITREOUS AND OCULAR PATHOLOGIES
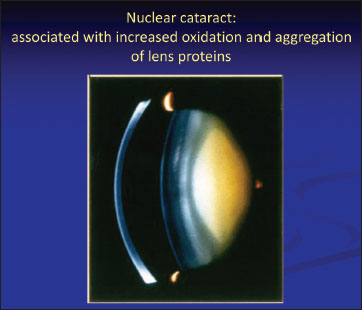
Oxygen and Nuclear Sclerotic Cataract The crystalline lens exists in a hypoxic state thought to be essential for lens clarity. It is well established that age-related or nuclear sclerotic cataract is caused by oxidative damage to the nuclear proteins in the lens (Figure 4). Although the final damage-causing step may involve free radical oxygen species, the source is molecular oxygen diffusing from the vascularized tissues of the eye.
LOOKING TO THE FUTURE
If vitreous liquefaction represents an early step in the pathogenesis of nuclear cataract and some cases of open angle glaucoma, perhaps research efforts should focus on preventing vitreous liquefaction. Currently, there is far more interest in pharmacologic vitreolysis. Perhaps the field of retina, and all of ophthalmology, would benefit from doing exactly the opposite: preventing vitreous liquefaction and posterior vitreous detachment. The possible benefits of being able to maintain a vitreous gel throughout life are many: no nuclear sclerotic cataracts, reduced cases of open angle glaucoma, and reduced cases of retinal tears, retinal detachments, macular holes, vitreomacular traction, macular pucker, bleeding from proliferative diabetic retinopathy, etc. The list goes on. Unfortunately, there is currently very little understanding of the mechanism of vitreous liquefaction and very few research efforts in this area. The importance of a gel vitreous to the health of the eye has long been unexamined. Vitreous research is the unexplored frontier of the eye. I am sure the vitreous gel will continue to surprise us. RP
REFERENCES
1. Shui YB, Holekamp NM, Kramer BC, et al. The gel state of the vitreous and ascorbate-dependent oxygen consumption: relationship to the etiology of nuclear cataract. Arch Ophthalmol. 2009; 127:475-482. 2. Holekamp NM, Shui YB, Beebe DC. Vitrectomy surgery increases oxygen exposure to the lens: a possible mechanism for nuclear cataract formation. Am J Ophthalmol. 2005; 139:302-310. 3. Siegfried CJ, Shui YB, Holekamp NM, Bai F, Beebe DC. Oxygen distribution in the human eye: relevance to the etiology of open-angle glaucoma after vitrectomy. Invest Ophthalmol Vis Sci. 2010; 51:5731-5738. 4. Chang S. LXII Edward Jackson lecture: open angle glaucoma after vitrectomy. Am J Ophthalmol. 2006; 141:1033-1043.