Vitreous: The Next Frontier
Source: http://retinatoday.com/2016/06/vitreous-the-next-frontier/
Vitreous liquefaction is the cause of many age-related ocular diseases. Figuring out its cause—and how to prevent it—could help to preserve eye health. By Nancy M. Holekamp, MD
The vitreous humor is the root of all evil. That may not exactly be true, but I hope this article will convince you that vitreous liquefaction is the root cause of many ocular disorders, and that an intact vitreous gel is essential to the health of the human eye. Accordingly, the vitreous merits our profession’s attention as the next frontier for scientific research. To begin, let us take a moment to discuss the vitreous body.
AT A GLANCE
• An intact vitreous gel is essential to the health of the eye.
• Vitreous liquefaction occurs with age, and diseaserelated sequelae can include retinal tears, retinal detachment, vitreomacular traction, macular pucker, macular hole, and bleeding from retinal neovascularization as well as nuclear sclerotic cataract and increased risk of primary open-angle glaucoma.
• Preventing vitreous liquefaction might enable individuals to retain the healthy eyes of youth.
THE VITREOUS, IN BRIEF
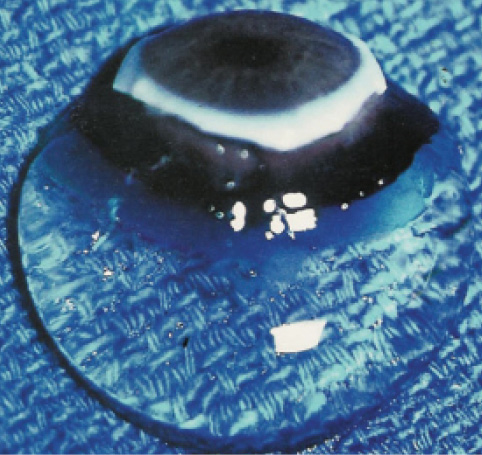
When we are born, most of the eye’s interior is filled with the vitreous body, which is 100% gel-like in structure and optically clear so we are able to see through it (Figures 1 and 2). Around the age of 9 or 10, the human vitreous gel begins to liquefy, and it continues to do so inexorably throughout one’s life.1 Once an individual reaches advanced age, little vitreous gel remains in the vitreous cavity. Instead, there is essentially an aqueous-like liquid in its place.
To review: children have an intact vitreous gel, whereas by adulthood the vitreous gel is constantly in the process of liquefaction. Pediatric ophthalmologists treat a completely different set of ocular disorders than do general ophthalmologists who treat adult patients. Taking these observations into consideration, could vitreous liquefaction have a bearing on age-related eye disease? The answer is “yes.”
VITREOUS LIQUEFACTION AND AGE-RELATED EYE DISEASE
Recent research has indicated that vitreous liquefaction induces age-related nuclear sclerotic cataract,2 which occurs as a result of the oxidation of proteins within the nucleus of the lens. The oxygen comes from the retina and choroid. The vitreous gel consumes molecular oxygen in an ascorbate-dependent manner, thus protecting the lens from oxidation. However, a liquefied vitreous loses the ability to consume oxygen, thus exposing the lens to excess oxidation, resulting in nuclear cataract. If a person lives long enough to develop extensive vitreous liquefaction, he or she will develop nuclear cataract.
Other research has pointed to vitreous liquefaction as being responsible for approximately 15% to 20% of primary open-angle glaucoma cases.3,4 As noted above, the vitreous gel consumes oxygen in an ascorbate-dependent manner, but the crystalline lens itself also consumes oxygen using mitochondria in the lens epithelium and reduced glutathione in the lens cortex. An aging eye with vitreous liquefaction that develops the expected nuclear cataract and undergoes cataract surgery loses two important means for regulating oxidative stress inside the eye: the vitreous gel and the lens. Consequently, intraocular oxygen tension in the eye rises, leading to oxidation of the trabecular meshwork, which leads to a recalcitrant form of open-angle glaucoma (think of aphakic glaucoma) that is refractory to medical therapy and often requires surgery.
Finally, every retina specialist is well-versed in the fact that vitreous liquefaction can cause retinal tears, retinal detachment, vitreomacular traction, macular pucker, macular hole, and bleeding from retinal neovascularization. These ocular disorders result from anomalous posterior vitreous detachment, defined by Sebag as “gel liquefaction in excess of the degree of vitreoretinal dehiscence.”5 It is the unifying concept in vitreoretinal disease.
WHY VITREOUS LIQUEFACTION?
In a perfect world, the vitreous gel would never liquefy, and most of what we general ophthalmologists and retina specialists operate on would not require surgical intervention. Furthermore, if the vitreous gel were never to liquefy, then perhaps our eyes would remain as healthy as they were when we were 7 or 8 years old.
The first step to preventing any disease state requires understanding its pathophysiology. Unfortunately, our current knowledge does not adequately explain what leads to vitreous liquefaction. There are, however, many hypotheses. Jerry Sebag, MD, FACS, FRCOphth, FARVO, believes that ultraviolet light causes protein structural degradation of the collagen fibrils and the extracellular matrix [personal communication]. Roger Truscott, PhD, believes the collagen in vitreous consists of long-lived proteins (ie, proteins that do not turn over during life). According to Truscott, body temperature causes those proteins to undergo slow degradation of structure and function (think of frying an egg at 30˚ over 20 years rather than at 300˚ in 2 minutes). Over a lifetime this leads to vitreous liquefaction [personal communication].
The Japanese literature is rife with theories on vitreous liquefaction that can generally be summarized as follows: the intraocular environment is a sea of cellular reactions that are continually occurring. This generates reactive oxygen species that denature hyaluronic acid, one of the main components of the vitreous gel structure.6,7
These are all good theories, but no one has studied and proved them.
PREVENTING VITREOUS LIQUEFACTION
Not only do we not know what causes vitreous liquefaction, but few scientists are involved in research to find out. At the recent meeting of the Macula Society in Miami, Florida, 143 scientific papers were presented, none of which were on the vitreous gel. There were no panels or papers on vitreous research at the American Academy of Ophthalmology Retina Subspecialty Day last year. Only the Euretina meeting consistently includes main sessions on vitreous physiology, thanks to the singular efforts of Einar Stefansson, MD, PhD, a long-time pioneer in the field. Have we been neglecting the vitreo– aspect of our vitreoretinal specialty?
A research group led by the late David C. Beebe, PhD, is studying the vitreous in collaboration with Purdue biomedical engineer Alyssa Panitch, PhD, who studies degradation or liquefaction of cartilage. Now headed by Ying-Bo Shui, MD, PhD, and Carl Siegfried, MD, at the Washington University School of Medicine in St. Louis, the research effort is using synthetic proteoglycan mimics to protect the vitreous gel structure from enzymatic degradation in vitro and in vivo.8 This team of researchers sought to determine whether it is possible to prevent or preserve the vitreous from degeneration.
We all know that the vitreous gel is 99% water and 1% solid and that the solid portion contains five types of collagen, hyaluronan, and proteoglycans. Applying a novel concept developed by Panitch, the researchers treated bovine vitreous in vitro with proteoglycan mimics targeting collagen, hyaluronan, or both. The bovine vitreous was then incubated overnight with trypsin. Enzymatic liquefaction of the pretreated vitreous was prevented, compared with untreated controls.
Furthermore, this research team utilized quick-freeze deep-etch electron microscopy to perform morphologic analysis. The structure of the pretreated vitreous gel was preserved when compared with controls. The proteoglycan mimics were shown to be well-tolerated in vivo when injected into porcine vitreous, with no histologic or electroretinographic changes to the retina. Proteoglycan mimics demonstrated the potential ability to maintain the gel-like structure of bovine vitreous, and no toxicity was observed when it was injected into the porcine eye. Of course, this work is in its infancy and requires further investigation on long-term toxicity, stability, and efficacy.
CONCLUSION
Retina specialists have been treating the complications of vitreous liquefaction rather than working to prevent the process. As a profession, we have overlooked the vitreous gel as an interesting and valuable area of study. Industry has recently brought us an agent to induce a posterior vitreous detachment9 when perhaps instead we should be preventing posterior vitreous detachment. If we could prevent vitreous liquefaction, and consequently prevent many age-related ocular diseases, then perhaps we could all retain the healthy eyes we had in our youth. n
1. Sebag J. The vitreous. In: Adler FH, Hart WM, eds. Adler’s physiology of the eye. 9th ed. St. Louis: Mosby; 1992:268-347.
2. Shui YB, Holekamp NM, Kramer BC, et al. The gel state of the vitreous and ascorbate-dependent oxygen consumption: relationship to the etiology of nuclear cataract. Arch Ophthalmol. 2009;127(4):475-482.
3. Chang S. LXII Edward Jackson lecture: open angle glaucoma after vitrectomy. Am J Ophthalmol. 2006;141(6):1033-1043.
4. Siegfried CJ, Shui YB, Holekamp NM, et al. Oxygen distribution in the human eye: relevance to the etiology of open angle glaucoma after vitrectomy. Invest Ophthalmol Vis Sci. 2010;51(11):5731-5738.
5. Sebag J. Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol. 2004;242(8):690-698.
6. Takahashi K, Arai K, Hayashi S, Tanaka Y. Degree of degraded proteoglycan in human vitreous and the influence of peroxidation. Nippon Ganka Gakkai Zasshi. 2006;110(3):171-179.
7. Akiba J, Yanagiya N, Kakehashi A, et al. Coppe-ion-catalyzed vitreous liquefaction in vivo. Ophthalmic Res. 1997;29(1);37-41.
8. Zhang Q, Filas BA, Roth R, et al. Preservation of the structure of enzymatically-degraded bovine vitreous using synthetic proteoglycan mimics. Invest Ophthalmol Vis Sci. 2014;55(12);8153-6812.
9. Varma R, Haller JA, Kaiser PK. Improvement in patient-reported visual function after ocriplasmin for vitreomacular adhesion: results of the microplasmin for intravitreous injection-traction release without surgical treatment trials. JAMA Ophthalmol. 2015;133(9);997-1004.
Nancy M. Holekamp, MD
• director of retina diseases, Center for Macular Degeneration, Pepose Vision Institute, in Chesterfield, Mo.
• financial interest: none acknowledged
• nholekamp@gmail.com